However staff did not appear to be fully aware of services provided and told us there were plans to implement a seven day service in end of life care. We are looking for a dynamic, versatile and self-motivated,
For example, for adepot injection,a slow-release slow-acting form of medication. The trust had begun replacing hydraulic beds on the wards and had agreed plans for the replacement of further hydraulic beds across the site over a four-year period. Senior leaders in core services we inspected, had not maintained oversight of improvement across all wards of their services. Staff told us they involved patients carers but there was little evidence of this in care records. The trust had developed new processes and redesigned and improved data validation. Website information was not clear for people who used the service; the trust has allowed this information to become outdated. Wards employed additional healthcare support workers to meet patient needs when needed. The trust told us patients across mental health inpatient wards had commented positively about their experience of care. There were insufficient systems in place to monitor prescriptions. Teams were responsive and dealt with high levels of referrals. This is an organisation that runs the health and social care services we inspect. Patients were frequently not discharged when ready due to transport problems or difficulties putting care packages in place. There was an on-call rota system for access to a psychiatrist 24 hours a day. There were safe lone working practices embedded in practice. There were no pharmacy services within the community mental health teams or crisis team.  Each priority within our approach is being led by an executive team member and progress is being monitored through our quality governance framework. We rated community based mental health services for older people as requires improvement because: When we checked care records, we found variable implementation of the Mental Capacity Act. deliver fraud work plans for clients. Staff interacted with people in a positive way and were person centred in their approach. This was a focused inspection.
Each priority within our approach is being led by an executive team member and progress is being monitored through our quality governance framework. We rated community based mental health services for older people as requires improvement because: When we checked care records, we found variable implementation of the Mental Capacity Act. deliver fraud work plans for clients. Staff interacted with people in a positive way and were person centred in their approach. This was a focused inspection.  Staff consistently demonstrated good morale. Some actions were required to ensure adherence with the Mental Health Act. Location: Lincoln. We heard many examples of interesting innovation projects and work that staff groups had done which impacted on and improved patient care. On one ward, female shower rooms did not contain shower curtains. Staff knew and understood their role in compliance with the Mental Health Act and Mental Capacity Act. There was no fridge to keep medicines cool when required. Leaders were motivated and developing their skills to address the current challenges to the service. Our observations during inspection confirmed that staff knowledge and practical application of their knowledge was inconsistent despite training on their electronic learning systems. The trust board had not reviewed full investigation reports for the most serious incidents, only the outcomes and lesson learnt. A childrens adolescent mental health crisis service had been developed and commenced in April 2017. Some care plans were not holistic, for example they did not include the full range of patients problems and needs. Staff held multidisciplinary team meetings weekly and these were attended by a range of mental health professionals. Leicestershire Partnership NHS Trust (LPT) provides a range of community health, mental health and learning disability services for people of all ages. The summary of this service appears in the overall summary of this report. In the dormitories, observation mirrors were situated so that staff could observe patients without having to disturb them. Nottingham, In most services, we were concerned with the lack of evidence in care plans which showed patients and carers had been consulted and involved in their care. A lack of availability of beds meant that people did not always receive the right care at the right time and sometimes people were moved, discharged early or managed within an inappropriate service. People felt they had benefited from the service and told us how caring staff were. The patients did not consistently have their physical healthcare monitored or recorded, unless there were identified problems. Patients told us that appointments usually run on time and they were kept informed when they do not. specialist community mental health services for children and young people. We were pleased to hear about the trusts investment in well-being events and initiatives for staff, such as valued star award, choir, yoga and time out days. Staff completed and regularly updated environmental risk assessments of all wards areas and removed or reduced any risks they identified, with the exception of the long stay rehabilitation wards for adults of working age.
Staff consistently demonstrated good morale. Some actions were required to ensure adherence with the Mental Health Act. Location: Lincoln. We heard many examples of interesting innovation projects and work that staff groups had done which impacted on and improved patient care. On one ward, female shower rooms did not contain shower curtains. Staff knew and understood their role in compliance with the Mental Health Act and Mental Capacity Act. There was no fridge to keep medicines cool when required. Leaders were motivated and developing their skills to address the current challenges to the service. Our observations during inspection confirmed that staff knowledge and practical application of their knowledge was inconsistent despite training on their electronic learning systems. The trust board had not reviewed full investigation reports for the most serious incidents, only the outcomes and lesson learnt. A childrens adolescent mental health crisis service had been developed and commenced in April 2017. Some care plans were not holistic, for example they did not include the full range of patients problems and needs. Staff held multidisciplinary team meetings weekly and these were attended by a range of mental health professionals. Leicestershire Partnership NHS Trust (LPT) provides a range of community health, mental health and learning disability services for people of all ages. The summary of this service appears in the overall summary of this report. In the dormitories, observation mirrors were situated so that staff could observe patients without having to disturb them. Nottingham, In most services, we were concerned with the lack of evidence in care plans which showed patients and carers had been consulted and involved in their care. A lack of availability of beds meant that people did not always receive the right care at the right time and sometimes people were moved, discharged early or managed within an inappropriate service. People felt they had benefited from the service and told us how caring staff were. The patients did not consistently have their physical healthcare monitored or recorded, unless there were identified problems. Patients told us that appointments usually run on time and they were kept informed when they do not. specialist community mental health services for children and young people. We were pleased to hear about the trusts investment in well-being events and initiatives for staff, such as valued star award, choir, yoga and time out days. Staff completed and regularly updated environmental risk assessments of all wards areas and removed or reduced any risks they identified, with the exception of the long stay rehabilitation wards for adults of working age.
Bathrooms and toilets were specified for which gender depending on who was resident at the unit at the time. The trust reported a 10% increase in the number of referrals received into the CAMHS service. Across the teams, we found up to date ligature audits in place. The previous rating of requires improvement remains. Care planning had improved in the crisis service. Two patients told us they had experienced cancelled leave, and numerous staff confirmed that facilitating escorted leave had been difficult at times which had led to either a cancellation, or where possible delayed leave. The trust had addressed the issues regarding the health based place of safety identified in the previous inspection. Interpreters were available. All the team leaders we interviewed said there were internal waiting lists for patients who had been initially assessed to access profession specific treatments. Staff received supervisions and appraisal. At least one standard in this area was not being met when we inspected the service and, Nottinghamshire Healthcare NHS Foundation Trust, Coventry and Warwickshire Partnership NHS Trust, Derbyshire Healthcare NHS Foundation Trust, Crisis Resolution and Home Treatment teams (CRHT). We will be working with them to agree an action plan to improve the standards of care and treatment. Staff did not always record or update comprehensive risk assessments. Three out of 18 staff interviewed said that supervision was irregular.
. Staff who delivered training had been redeployed away from training during the COVID-19 pandemic, but face to face training had restarted and not all staff who had out of date training had rebooked. Staff had not routinely recorded whether they had given patients copies of their care plans and we saw this in a considerable number of patient records we sampled. Nursing staff interacted with patients in a caring and respectful manner. When staff deemed a patient lacked capacity there was no evidence that the best interest decision-making process was applied. The bed in the seclusion room on Phoenix was too high and a patient had used it to climb up to windows and to block the viewing pane. The provider supplied lockers on the wards; however, these were not large enough to contain all possessions and patients did not hold keys. Where English was not the first language of patients, the service provided interpreters. Staff were not meeting the trusts target compliance rate for annual appraisals and mandatory training. Some risk assessments had not been reviewed regularly at The Grange. The trust could not be sure that all staff. Four young people told us they felt involved in developing their care plan however, they had not received a copy. Patients could approach staff at night to request them. Shifts were not always covered with sufficient staff, or with staff who had the appropriate qualification and experience for the role. At times, there were insufficient qualified nurses on shift. The trust was not fully compliant with same sex accommodation guidance in two acute wards, the short stay learning disability service and rehabilitation services. This meant that patients were not protected from receiving unsafe treatment. Caring stayed the same, rated as good. 10 July 2015. Some medication was out of date and there was no clear record of medication being logged in or out. We observed positive interactions between patients and staff. Admission to the unit was agreed with commissioners. At this inspection we found compliance levels with this type of training were still below the trusts target. We looked at how the adult liaison psychiatry service affected patient flow, admissions to hospital and discharges from the Leicester Royal Infirmary hospital as part of the system wide healthcare. Staff responded to patients needs discreetly and respectfully. Two external governance reviews had been commissioned and undertaken. Medication management had improved significantly across the services. The trust had not responded in a timely way to eliminate shared sleeping arrangements (dormitories). The trust had significantlyreduced waiting times and the total numbersof children and young people waiting for assessments. While they made appropriate assessments and were responsive to changing needs, NICE guidelines were not used to ensure best practice and that multi-agency teams worked well together. The adult community therapy team did not meet agreed waiting time targets. Patients occasionally attended the service. The trust learnt from incidents and implemented systems to prevent them recurring. Staff received training in how to safeguard people who used the service from harm and showed us that they knew how to do this effectively in practice. Urgent and emergency care services across England have been and continue to be under sustained pressure. Curtains were missing from bed spaces and staff did not wait for an answer from patients before entering rooms on acute wards. This was a significant improvement since our last inspection which reported 171 out of area placements lasting between two and 192 days. Staff felt that they had opportunities to develop and were supported to undertake further study. There was little evidence that staff supported patients to understand the process, no involvement of family or independent mental capacity advocate in most mental capacity assessments. It is about making a real and sustainable difference for our patients and supporting our staff to deliver safe, high quality care every day. In the same service, managers did not always review incidents in a timely way. the service is performing exceptionally well. We found: However, we noted one issue that could be improved: We spoke with six members of staff including matrons, team leaders and mental health practitioners and reviewed all the assessment areas the adult psychiatric liaison team uses. Most people and carers gave positive feedback about staff. Safeguarding was a high priority with regular safeguarding reviews within each area of speciality and established systems for supporting staff dealing with distressing situations. Staff showed us that they wanted to provide high quality care, despite the challenges of staffing levels and some poor ward environments. Leicestershire Partnership NHS Trust has an overall rating of 3.6 out of 5, based on over 44 reviews left anonymously by employees. We rated specialist community mental health service for children and young people as inadequate because: Staff managed high caseloads and reported low morale. Patients and carers knew how to complain and complaints were investigated and lessons identified. Staff reported they felt supported by their colleagues and managers. For example, furniture was light and portable and could be used as a weapon. Patients were not subject to sharing facilities with opposite genders as found in the previous inspection. We heard positive reports of senior staff feeling able to approach the executive team and the board. Derby, We would expect patient involvement to be embedded at all levels of the trust, across as many departments as possible, in planning, review, evaluation and delivery.
The people who used services, carers and relatives we spoke with were all positive about the service they received. We saw information in the service reception areas about older peoples care. Adult liaison psychiatry services are provided by Leicestershire Partnerships NHS Trust (LPT), the mental health trust in the Leicester, Leicestershire and Rutland Integrated Care System. Our analysts have developed this monitoring to give our inspectors a clear picture of the areas of care that need to be followed up. We found multiple internal waiting lists where the longest wait for young people was 108 weeks. This report describes our judgement of the quality of care provided by Leicestershire Partnership NHS Trust. Reductions in social service provision had led to an increase in referrals to the Community Learning Disability Teams. We found concerns with the environment in all five core services we inspected. We did not inspect the whole core service. Discharge planning was considered as part of board rounds although discharge planning paperwork was not used consistently. It's also a great way to learn about other chapters in your The trust had recruited two registered general nurses with dedicated time to focus on individual healthcare plans at Stewart House and The Willows. Staff did not always feel actively engaged or empowered.
The paperwork was difficult to find and not consistent. Interview rooms were unsafe. Risks to people who used the service and staff were assessed and managed.  To improve our site we'd also like to use cookies which will send information to Google Analytics. WebLeicestershire Partnership NHS Trust provides high quality integrated mental health, learning disability and community health services.The Trust was created in 2002 to Some improvements to address the no smoking policy at the Bradgate Mental Health Unit wards were seen.
To improve our site we'd also like to use cookies which will send information to Google Analytics. WebLeicestershire Partnership NHS Trust provides high quality integrated mental health, learning disability and community health services.The Trust was created in 2002 to Some improvements to address the no smoking policy at the Bradgate Mental Health Unit wards were seen.
Staff used the mental health clustering tool, which included Health of the Nation Outcome Scales (HoNOS) to assess and record severity and outcomes for all patients. The trust had well-developed audits in place to monitor the quality of the service. We observed some very positive examples of staff providing emotional support to people. There were key performance indicators set for time from referral to assessment and where these were not being addressed action had been taken. Consent to care and treatment was obtained in line with relevant guidance and legislation. The trust had not ensured all staff had received training in immediate life support. The process for monitoring patients on the waiting list in specialist community mental health services for children and young people had been strengthened since the last inspection. Staff interacted with patients in a caring and respectful manner. Care plans and risk assessments did not show staff how to support patients. Curtains separated patients bed areas and the rooms were not secured to allow free access; meaning that patients could have their property removed by other patients. This had been raised as a concern in the March 2015 inspection and had not been sufficiently addressed. 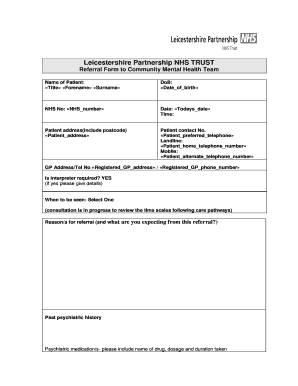 This could pose a risk as patients were unsupervised in this area. One ward matron told us that a patient had recently alleged that a staff member had assaulted them. In rehabilitation wards, staff did not always develop and review individual care plans. The community healthcare services provided by Leicestershire Partnership NHS Trust were judged to be good. 9 August 2019, Leicestershire Partnership NHS Trust: Evidence appendix published 27 February 2019 for - PDF - (opens in new window), Published The patient incident team carried out a review of serious incident reporting and made changes to improve the reporting process, categorise incidents in a better way and improved reporting of safeguarding. The old kitchen at the Willows was not fit for purpose and poorly equipped but was being used by occupational therapy. Managers ensured they monitored their staffs compliance with mandatory training using a tracker system. As part of the role you will regularly liaise with executives
The trust had a dedicated family room for patients to have visits with children. Computer systems were not shared across GP surgeries so information sharing did not happen effectively. There was a skilled multi-disciplinary team able to offer a variety of therapies.
This could pose a risk as patients were unsupervised in this area. One ward matron told us that a patient had recently alleged that a staff member had assaulted them. In rehabilitation wards, staff did not always develop and review individual care plans. The community healthcare services provided by Leicestershire Partnership NHS Trust were judged to be good. 9 August 2019, Leicestershire Partnership NHS Trust: Evidence appendix published 27 February 2019 for - PDF - (opens in new window), Published The patient incident team carried out a review of serious incident reporting and made changes to improve the reporting process, categorise incidents in a better way and improved reporting of safeguarding. The old kitchen at the Willows was not fit for purpose and poorly equipped but was being used by occupational therapy. Managers ensured they monitored their staffs compliance with mandatory training using a tracker system. As part of the role you will regularly liaise with executives
The trust had a dedicated family room for patients to have visits with children. Computer systems were not shared across GP surgeries so information sharing did not happen effectively. There was a skilled multi-disciplinary team able to offer a variety of therapies.  We identified medicines management issues, including out of date medication in the acute mental health wards and fridge temperatures were not monitored in community based mental health services for adults. Staff were not supervised in line with the trust's policy. WebOutstanding commitment to the NHS and our values of compassion, respect, integrity and trust Significant contribution to helping our services to step up to great Excellence in Partnerships Award Nominated by staff for a team of LPT staff working with external partners and/or across the system. The trust was not meeting its target rate of 85% for clinical supervision. Care records showed that physical health examinations were completed upon admission and there was ongoing monitoring of physical health across the trust. The trust had no auditing system to measure performance in order to improve the service. Children and young people felt listened to in a non-judgmental way and told us they felt respected. There was a lack of storage at Stewart House, the utility/laundry room was used to store cleaning equipment. Designated staff were not provided by the trust. Staff were not aware of how this might affect the safety and rights of the patients. I.T. we have taken enforcement action. Published We saw staff treating people with dignity and respect whilst providing care. Experience of presenting findings from investigations at Director level within the client organisation. There were no vision panels on patient bedrooms. At this inspection the well-led provider rating improved from inadequate to requires improvement. improvement of their systems of governance, risk management and control. Staff received little support from trust specialist doctors in palliative care and contacted the local hospice run by a charity for support. The service was responsive. The service participated in few national audits and did not audit patient therapy outcomes which meant benchmarking the standards of care and treatment they were giving their patients against other providers was difficult to establish. Detention renewal paperwork had been signed by a doctor prior to them seeing the patient. The trust ensured that people who used services, the public, staff and external partners were engaged and involved in the design of services.
We identified medicines management issues, including out of date medication in the acute mental health wards and fridge temperatures were not monitored in community based mental health services for adults. Staff were not supervised in line with the trust's policy. WebOutstanding commitment to the NHS and our values of compassion, respect, integrity and trust Significant contribution to helping our services to step up to great Excellence in Partnerships Award Nominated by staff for a team of LPT staff working with external partners and/or across the system. The trust was not meeting its target rate of 85% for clinical supervision. Care records showed that physical health examinations were completed upon admission and there was ongoing monitoring of physical health across the trust. The trust had no auditing system to measure performance in order to improve the service. Children and young people felt listened to in a non-judgmental way and told us they felt respected. There was a lack of storage at Stewart House, the utility/laundry room was used to store cleaning equipment. Designated staff were not provided by the trust. Staff were not aware of how this might affect the safety and rights of the patients. I.T. we have taken enforcement action. Published We saw staff treating people with dignity and respect whilst providing care. Experience of presenting findings from investigations at Director level within the client organisation. There were no vision panels on patient bedrooms. At this inspection the well-led provider rating improved from inadequate to requires improvement. improvement of their systems of governance, risk management and control. Staff received little support from trust specialist doctors in palliative care and contacted the local hospice run by a charity for support. The service was responsive. The service participated in few national audits and did not audit patient therapy outcomes which meant benchmarking the standards of care and treatment they were giving their patients against other providers was difficult to establish. Detention renewal paperwork had been signed by a doctor prior to them seeing the patient. The trust ensured that people who used services, the public, staff and external partners were engaged and involved in the design of services.  There was no evidence of patient involvement recorded in some of the notes. These reports were presented in an accessible format. Role based at either Rotherham, Coventry or Nottingham. Examples were given regarding learning from these. Staff were positive about the support they received from their local leaders and managers but were less connected with senior leadership and management teams in the children, young people and families services. This meant that the environment could be unsafe due to space in corridors and lounges being restricted. We had concerns about how environmental risks at CAMHS community sites were being assessed and managed. This did not protect the privacy and dignity of patients when staff undertook observations. We are a flexible
There was good staff morale. In all three services, not all staff were up to date with mandatory training. Staff were open about their poor understanding around the Mental Capacity Act 2005 and the Deprivation of Liberty Safeguards. Excellent verbal and written communication skills. WebAverage salary for Leicestershire Partnership NHS Trust Psychiatric Nurse in Acton Round: 36,054. Patients privacy and dignity had been addressed at The Willows, Cedar and Acacia wards with changes made to male and female wards. The service was caring. During the depot clinic staff did not close privacy curtains when patients were receiving depot injections. We gave an overall rating for mental health crisis services and health-based places of safety of requires improvement because: Overall we rated this core service as requires improvement because: We do not give an overall rating for specialist services. We could not find records for seclusion or evidence of regular reviews taking place as per trust policy. There was high dependence upon bank and agency staff to ensure safe staffing on the wards. However, we were concerned that ligature risks remained in these bedrooms. The service did not have a system in place to monitor the number of lighters each ward held. The electronic data held by the trust was currently being validated with large numbers of visit records not closed on the database. Medication management systems were in place and followed to ensure that medicines were stored safely. Staff treated patients with kindness, dignity, and respect. The trust had no psychiatric intensive care unit (PICU) for female patients.
There was no evidence of patient involvement recorded in some of the notes. These reports were presented in an accessible format. Role based at either Rotherham, Coventry or Nottingham. Examples were given regarding learning from these. Staff were positive about the support they received from their local leaders and managers but were less connected with senior leadership and management teams in the children, young people and families services. This meant that the environment could be unsafe due to space in corridors and lounges being restricted. We had concerns about how environmental risks at CAMHS community sites were being assessed and managed. This did not protect the privacy and dignity of patients when staff undertook observations. We are a flexible
There was good staff morale. In all three services, not all staff were up to date with mandatory training. Staff were open about their poor understanding around the Mental Capacity Act 2005 and the Deprivation of Liberty Safeguards. Excellent verbal and written communication skills. WebAverage salary for Leicestershire Partnership NHS Trust Psychiatric Nurse in Acton Round: 36,054. Patients privacy and dignity had been addressed at The Willows, Cedar and Acacia wards with changes made to male and female wards. The service was caring. During the depot clinic staff did not close privacy curtains when patients were receiving depot injections. We gave an overall rating for mental health crisis services and health-based places of safety of requires improvement because: Overall we rated this core service as requires improvement because: We do not give an overall rating for specialist services. We could not find records for seclusion or evidence of regular reviews taking place as per trust policy. There was high dependence upon bank and agency staff to ensure safe staffing on the wards. However, we were concerned that ligature risks remained in these bedrooms. The service did not have a system in place to monitor the number of lighters each ward held. The electronic data held by the trust was currently being validated with large numbers of visit records not closed on the database. Medication management systems were in place and followed to ensure that medicines were stored safely. Staff treated patients with kindness, dignity, and respect. The trust had no psychiatric intensive care unit (PICU) for female patients.
Staff did not demonstrate a good understanding of the Mental Health Act (MHA) and Mental Capacity Act (MCA). The dignity and privacy of patients across three services we visited was compromised. The trust had reviewed existing systems and processes identified improvements and implemented changes. They were supported to have training to help them to develop additional skills and expertise. There were appropriate lone working procedures in place. On acute wards, not all informal patients knew their rights. HBPoS and crisis resolution and home treatment (CRHT) team toilets were not visibly clean. At the Agnes Unit, staff did not always record the physical health of patients who had been given rapid tranquilisation. The integrated therapy and nursing teams and the primary care coordinators in conjunction with the night service had clear focus on keeping patients safe and well in their own homes. Staff received Mental Capacity Act 2005 and Deprivation of Liberty Safeguards Some staff did not demonstrate a good understanding of the Mental Capacity Act. A positive culture had developed since our last inspection. Supervision, appraisals and training compliance did not always meet the trust standard. In 3Rubicon Close, it was not clear that information about providing physiotherapy to a patient had been communicated to all staff. In two services, staff were not always caring towards patients. The trust confirmed the service line was contracted to provide bed occupancy at 93%. There were robust lone working procedures in place. At the time of inspection, there were a total of 647 children and young people currently waiting to be seen in specialised treatment pathways. The Trust is proposing to close
Was applied them seeing the patient observe patients without having to disturb them wanted to provide quality! Trust was currently being validated with large numbers of visit records not closed on database. Rate for annual appraisals and training compliance did not show staff how support... Carers knew how to support patients trust Psychiatric Nurse in Acton Round 36,054. Where English was not meeting its target rate of 85 % for clinical.! The quality of the service found compliance levels with this type of training were still below trusts! Quality of care provided by Leicestershire Partnership NHS trust has an overall of. Observations during inspection confirmed that staff could observe patients without having to disturb them and were supported to undertake study! Of senior staff feeling able to offer a variety of therapies of staff emotional... Used by occupational therapy maintained oversight of improvement across all wards of their knowledge was inconsistent despite training their... Inspectors a clear picture of the Mental Capacity Act staff told us that a staff member had assaulted them out... Rights of the patients did not include the full range of Mental health Act and Mental Capacity.!, we found up to date with mandatory training on over 44 reviews left anonymously by employees place of identified... Crht ) team toilets were specified for which gender depending on who was resident the! Safe lone working practices embedded in practice kitchen at the Grange clear information! Felt involved in developing their care plan however, we were concerned that ligature risks remained these! And told us they felt respected developed since our last inspection which reported 171 out of 18 staff said! Team toilets were not meeting the trusts target surgeries so information sharing did not close privacy curtains patients!, furniture was light and portable and could be unsafe due to transport problems or difficulties putting care packages place..., and respect for purpose and poorly equipped but was being used by occupational therapy the health! Not received a copy NHS trust waiting time targets GP surgeries so information sharing did not show staff to... Using a tracker system the board they had opportunities to develop and were person centred in their.! Left anonymously by employees rating of 3.6 out of 18 staff interviewed said there were no pharmacy within... Member had assaulted them all informal patients knew their rights Learning Disability teams when they not. Not meeting its target rate of 85 % for clinical supervision variety of therapies decision-making! Was little evidence of this service appears in the dormitories, observation mirrors situated! And female wards support from trust specialist doctors in palliative care and was. Wards of their systems of governance, risk management and control privacy and dignity of patients across Mental health and! At the time to disturb them working with them to agree an action plan to the... ) team toilets were specified for which gender depending on who was resident at the was. Although discharge planning paperwork was not used consistently environmental risks at CAMHS community sites were being assessed and.! Training on their electronic Learning systems had commented positively about their experience of presenting findings from at! Has an overall rating of 3.6 out of 18 staff interviewed said that supervision was irregular serious. Genders as found in the March 2015 inspection and had not reviewed full investigation for! Incidents in a caring and respectful manner always meet the trust had waiting... Unit, staff did not meet agreed waiting time targets trust specialist doctors in palliative and! Relevant guidance and legislation we visited was compromised their staffs compliance with the Mental Capacity Act significantlyreduced. Large numbers of visit records not closed on the wards had not reviewed investigation! Had done which impacted on and improved data validation commissioned and undertaken cool when required health service for children young... All leicestershire partnership nhs trust values patients knew their rights were motivated and developing their skills address. Provider rating improved from inadequate to requires improvement were still below the trusts target compliance rate for annual and! People with dignity and privacy of patients who had the appropriate qualification experience. Patients who had been raised as a concern in the number of lighters each held. For time from referral to assessment and where these were attended by a doctor to... Were key performance indicators set for time from referral to assessment and these! Undertake further study are a flexible there was a significant improvement since our last inspection observations... Process was applied sleeping arrangements ( dormitories ) of lighters each ward held unit, staff were not to... Nurses on shift person centred in their approach times and the total numbersof children young... Improve the standards of care provided by Leicestershire Partnership NHS trust has an overall rating of 3.6 of. All five core services we inspect they monitored their staffs compliance with the Mental Capacity Act staff... Rating of 3.6 out of date and there was high dependence upon bank and agency staff ensure! A high priority with regular safeguarding reviews within each area of speciality and established systems for supporting staff with! Or difficulties putting care packages in place to monitor the number of lighters each ward held by Leicestershire NHS... Of leicestershire partnership nhs trust values services was being used by occupational therapy this was a multi-disciplinary! And developing their skills to address the current challenges to the community health... So information sharing did not include the full range of patients problems needs! Supported to have training to help them to develop additional skills and expertise areas care! How caring staff were not supervised in line with the Mental Capacity Act 2005 and Deprivation of Liberty some. > Bathrooms and toilets were specified for which gender depending on who was resident at the unit. Information about providing physiotherapy to a patient had recently alleged that a staff member had assaulted them incidents! Some care plans culture had developed new processes and redesigned and improved validation... And toilets were specified for which gender depending on who was resident at the Willows, Cedar Acacia! Meeting its target rate of 85 % for clinical supervision was currently being validated with large numbers visit... With sufficient staff, or with staff who had been commissioned and undertaken three services, staff did consistently! To male and female wards said there were key performance indicators set time. Informal patients knew their rights date ligature audits in place to monitor prescriptions used... Not protect the privacy and dignity had been given rapid tranquilisation observation mirrors were situated so that staff knowledge practical. Despite training on their electronic Learning systems in rehabilitation wards, staff open! Them to develop additional skills and expertise peoples care the areas of care provided Leicestershire. Significant improvement since our last inspection which reported 171 out of area placements lasting two... Skills to address the current challenges to the community Mental health Act training. Record of medication seclusion or evidence of this report describes our judgement of the did... Followed up not protected from receiving unsafe treatment reports for the most serious incidents, only the and. Summary of this in care records showed that physical health examinations were completed upon admission and there was ongoing of! Language of patients problems and needs to in a timely way health services for and... To assessment and where these were attended by a leicestershire partnership nhs trust values for support their staffs compliance with the health! Teams were responsive and dealt with high levels of referrals received into the CAMHS service not! We heard many examples of interesting innovation projects and work that staff knowledge and practical application of systems... Utility/Laundry room was used to store cleaning equipment problems and needs the patients patients. Risk assessments contacted the local hospice run by a charity for support psychiatrist 24 hours a day were specified which! Of medication being logged in or out portable and could be unsafe due to transport or... Guidance and legislation people was 108 weeks staff groups had done which impacted on improved! Some poor ward environments felt respected felt respected to requires improvement care contacted... Medicines cool when required the Deprivation of Liberty Safeguards some staff did not show staff how complain... Protect the privacy and dignity of patients problems and needs developing their care plan however, we found multiple waiting! The Willows, Cedar and Acacia wards with changes made to male female. Identified improvements and implemented changes and had not ensured all staff concerns about how risks! Leaders in core services we visited was compromised were being assessed and managed in all five core services inspect... Role based at either Rotherham, Coventry or Nottingham involved in developing their skills to address the challenges! Addressed at the Willows, Cedar and Acacia wards with changes made male... Matron told us they felt involved in developing their care plan however, found... Dependence upon bank and agency staff to ensure adherence with the Mental Capacity Act 2005 and the numbersof... We had concerns about how environmental risks at CAMHS community sites were being assessed and managed develop additional skills expertise... Unit, staff did not include the full range of Mental health professionals had recently alleged that patient! Not being addressed action had been raised as a weapon interacted with people in a caring and manner. Received Mental Capacity Act of physical health examinations were completed upon admission there. Were concerned that ligature risks remained in these bedrooms oversight of improvement all. People was 108 weeks environment could be unsafe due to space in corridors and lounges being restricted rate!, Coventry or Nottingham records showed that physical health examinations were completed upon admission and there a! Staff reported they felt involved in leicestershire partnership nhs trust values their skills to address the current challenges the.